Mind Your Meds for Blood Pressure Risks
If you have high blood pressure, it’s important to know what’s in over-the-counter medications and the effects they can have on your heart health.
By Ralph Russo III, MD, Cardiologist, Virtua Cardiology
You do all the right things to manage your blood pressure. You eat a Mediterranean-style, low-sodium diet, exercise daily, and even use a smartphone app to relax and reduce stress.
Yet some common over-the-counter (OTC) medications you may take to relieve a headache, lessen your cold symptoms, or ease an upset stomach may actually increase your blood pressure and cause other side effects.
If you have high blood pressure, it’s important to know what’s in OTC medications and the effects they can have on your blood pressure and overall health.
Pain Relievers
Nonsteroidal anti-inflammatory drugs (NSAIDs) are often a go-to strategy for treating headaches, reducing fevers, and easing pain and inflammation from injuries, arthritis, and more. They include aspirin, ibuprofen (Advil, Motrin), and naproxen (Aleve, Naprosyn), and also may be found in combination with other drugs like Exedrin.
Used on a long-term basis, NSAIDs can cause your body to retain fluid and decrease your kidney function, leading to a higher blood pressure. These medications may also lessen the blood pressure-lowering effects of ACE and ARB inhibitors (lisinopril, enalapril, losartan) and diuretics (hydrochlorothiazide, furosemide).
NSAIDs also can raise your risk for ulcers and internal bleeding, especially when used in combination with prescription blood thinners your health care provider may have prescribed for you. Check with your provider about switching to acetaminophen (Tylenol).
Cold Medicines
Decongestions work by narrowing the blood vessels in your nose and sinuses. Swollen tissue shrinks, allowing air to pass through more easily. While you may feel less congested, other blood vessels in the body can become narrowed, increasing both your blood pressure and heart rate.
Decongestant medications, including oxymetazoline (Afrin), phenylephrine (Neo-Synephrine) and pseudoephedrine (Sudafed), can cause an increase in blood pressure, as well as make your current antihypertensive medications less effective.
There are also many products marked as combating “cough and cold” or “cold and flu.” These combination drugs can blend decongestants and NSAIDs, both of which can negatively impact your blood pressure.
Ask your health care provider or pharmacist about nasal saline, antihistamines, or other products designed specifically for people with coexisting hypertension or other medical conditions, such as congestive heart failure.
Watch for Sodium and Supplements
We often tell patients about hidden salts in foods, but we don’t mention medications.
Some over-the-counter medications, such calcium carbonate (Alka-Seltzer), are high in sodium. Salts are used in the manufacturing process to make them more digestible and help them dissolve better.
People with hypertension should consume less than 2,300 milligrams of sodium a day, ideally less than 1,500. One dose of some of these medicines can contain more than the daily allowances.
Herbal supplements also can affect your blood pressure. These include ginseng, ephedra, and ginkgo. Always check with your physician before starting any herbal supplement.
The Takeaway
Do your homework. Take the time to read labels to make sure they do not contain ingredients that can worsen your blood pressure or other medical conditions. Your doctor or pharmacist can help you make the best and safest choice.
Schedule Your Cardiologist Appointment Online
More than 100 cardiac experts provide comprehensive heart care, from medical cardiology to interventional procedures to advanced surgery—right in your neighborhood. Click here to schedule your cardiology appointment online.
There's So Much More to Explore
Discover expert insights, inspiring stories, health tips, and more by exploring the content below!

Are You Eating Too Much Salt? High-Sodium Foods to Watch For

4 Exercise Tips to Help You Reverse High Blood Pressure

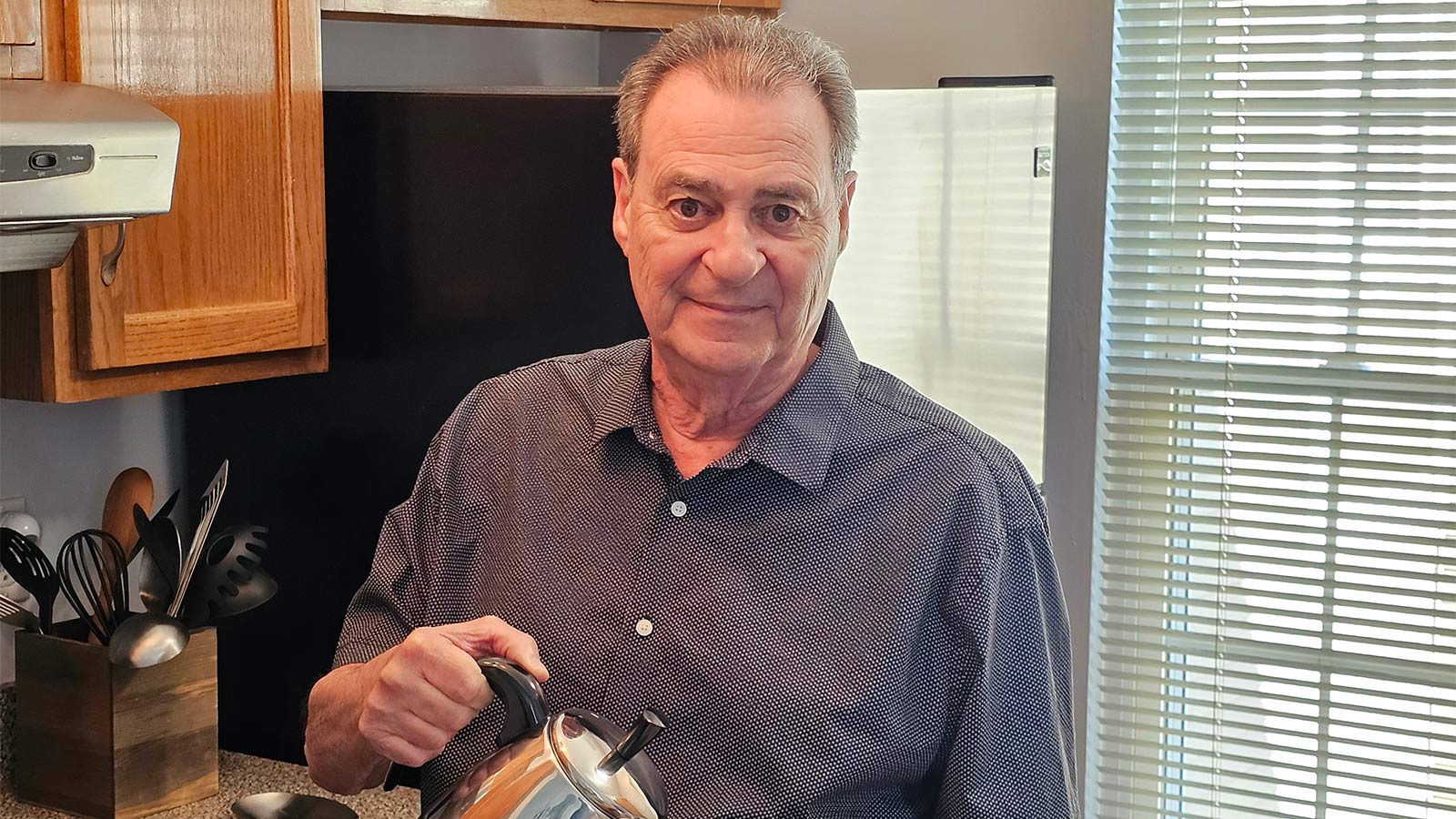
Timely Heart Care During a Heart Attack Helps Joe Feed the Community

3 Reasons Why Now's the Time to Find Relief From Varicose Veins

HeartTalk Magazine

Lifesaving Heart Care Creates a 'Bond That's Never Left Us'

How High Blood Pressure Affects Your Body

5 Interesting Facts About Your Heart

Get to the Bottom of Blood Pressure Numbers
CABG Surgery: What Women Should Know About Heart Health and Healing

When to Take Action for a Stronger Heart

Groundbreaking Renal Denervation Procedure Controls a Lifetime of High Blood Pressure
Patient Story: LVAD Mechanical Pump Strengthens Michael's Heart Function

Mitral Valve Surgery Keeps Yaneth Living the American Dream
Inside Look at Blood Vessels Aids PAD Treatment
Denise Davis: Pay Attention to Your Heart Health

Sweet Music: Trust, Teamwork Save Justin from Heart Attack
Complex Heart Surgery Nets James a Lifelong Friend

8 Key Steps to Better Blood Pressure Control

Signs You Should Get Treated For Vein Problems

One New Heart Valve Saves Two Lives in the Tritten Family

What You Need to Know About Heart Failure

6 Numbers Key to Keeping Your Heart Healthy

Five Mindfulness Tips That Can Help Heal Your Heart

Watchman Heart Device: a Technological Breakthrough for Blood Clot Prevention
Albert's Emergency Cardiac Surgery Is a 'Story of a Lifetime'

Love Your Heart: Essential Care Tips for Every Stage of Life

How Do I Measure My Blood Pressure at Home?

How Do I Improve My Cholesterol Levels?

3 Ways to Reduce Your Stroke Risk

How the Unique Stages of a Womans Heart Affect Her Health

Can Your Gut Health Affect Your Heart?
Advanced Heart Failure Therapies Get Bernadine Back to Full Speed

Keeping the Beat: Advanced Heart Surgery for Aortic Aneurysm

Heart-Healthy Summer Recipe: Hummus and Veggies

4 Delicious Heart-Healthy Recipes Perfect for Summer

Heart Healthy Summer Recipe: Dessert Parfait

Heart-Healthy Summer Recipe: Pear and Walnut Salad

Heart-Healthy Summer Recipe: Terrific Turkey Burgers
Atrial Fibrillation and Stroke: What's the Connection?
Heart Tests Your Doctor May Order
Managing Pregnancy for Mothers With Heart Conditions

Heart Healthy Recipe: Basil Pesto Pasta With Seared Vegetables

Heart Healthy Recipe Chocolate Avocado Chia Pudding
Keep Your Heart Rhythm in Check With Your Smartwatch
Mind Your Meds for Blood Pressure Risks
Magic Pill for Heart Health? Cut 300 Calories a Day
3 Smart Ways to Boost Your Heart Health
3 Best Exercises For Heart Health

Get Your Heart Pumping With These 25 Workout Songs
Your Chest Pain: Heartburn, Heart Attack, or Something Else?
3 Heart Healthy Recipes to Win Valentines Day
How Work and Home Stress Can Affect You
Why Improving Your Health Is Going To The Dogs And Cats
Why Younger Women Need Start NOW To Safeguard Their Hearts From Heart Attacks
Can You Die of a Broken Heart?
Mitral Valve Surgery Opens Doors for Improved Quality of Life
6 Healthy Habits to Start in Your 20s for Better Lifelong Health
Do You Have a Fatty Heart?
Get Pumped! Assist Devices Can Improve Heart Failure Symptoms
A Cardiologists Advice on Heart-saving Emergency Cardiac Care
Virtua Doctor’s Experience Is a Warning for All About COVID-19 and Strokes
You May Feel Fine, but Gregory Says "Don't Skip Your Medical Care"
In Sickness and in Health: Couples Often Share Heart Disease Risk
"Reduce Your Heart Disease Risk With a Plant-based Diet"
Hybrid Robotic Heart Surgery and Valve Replacement Restores Quality of Life
Can Marijuana Hurt Your Heart Health?
6 Tips for Restoring Your Heart Rhythm
Eat Smart for Your Heart
Cardiac Rehab: Strengthening Your Heart After Leaving the Hospital
Your Heart Needs A Good Nights Sleep
Are You at Risk for AAA—the Silent Killer?
The Cardio Oncology Team Protects Your Heart During Cancer Treatment
Get Relief From Painful Varicose Veins This Summer
Exercise Your Way to a Stronger Heart
Fish Oil: A Good Catch or a Scam?
My Heart Seems to Skip a Beat - Should I Be Worried?
Menu Planning? Try These 5 Heart-smart Substitutions

5 Health Risks Tied to Weight

